How Capital Surgeons Group is Redefining General Surgery
Surgery can be stressful — large incisions, extended hospital stays, and long recoveries can feel overwhelming. Capital Surgeons Group is changing that. Our expert surgeons combine decades of experience with advanced robotic, laparoscopic, and endoscopic techniques to make surgery safer, less invasive, and easier on patients’ lives.
Whenever possible, we perform minimally invasive procedures in 70–85% of eligible cases, helping patients experience smaller incisions, less pain, faster recovery, and lower complication rates. Peer-reviewed studies show that minimally invasive surgery reduces post-operative pain, lowers infection risk, and shortens hospital stays compared with traditional open surgery. When open surgery is necessary, our team ensures the safest, most effective approach — because at Capital Surgeons Group, your safety and outcomes always come first.
Robotic Hernia Surgery
Precision Where It Matters Most
Hernias can be uncomfortable and even painful, but proper repair restores comfort and prevents serious complications like bowel obstruction. Robotic hernia surgery offers enhanced precision, 3D visualization, and improved suturing for complex or recurrent hernias.
Learn more and schedule a consultation: Robotic Hernia Surgery
Colon, Abdominal & Intestinal Surgery
Advanced Care for Serious Conditions
Conditions such as colon cancer, diverticulitis, Crohn’s disease, and intestinal obstruction require specialized surgical care. Modern minimally invasive and robotic techniques treat these conditions effectively while reducing pain, hospital stays, and recovery time.
Learn more: Colon & Abdominal Surgery Services
GERD & Acid Reflux Surgery
Relief That Lasts
Severe GERD or hiatal hernia can significantly impact quality of life. When medications aren’t enough, surgical options such as laparoscopic fundoplication or hiatal hernia repair can provide lasting relief. Minimally invasive and robotic-assisted techniques make these procedures safer, precise, and easier to recover from.
Learn more: GERD & Acid Reflux Surgery
Endocrine Surgery
Thyroid, Parathyroid & Adrenal Care
Disorders of the thyroid, parathyroid, and adrenal glands require careful surgical management. Minimally invasive techniques reduce recovery time while maintaining precision and safety.
Learn more: Endocrine Surgery Services
Gallbladder & Liver Surgery
Modern Techniques for Complex Organs
Diseases of the gallbladder and liver range from gallstones to complex tumors, requiring precise surgical care. Minimally invasive and robotic techniques allow many patients to undergo these procedures safely, with smaller incisions and faster recovery.
Learn more: Gallbladder & Liver Surgery
Breast Disease, Biopsy & Surgery
Safety Meets Cosmetic Care
Breast conditions, benign or malignant, require precision and cosmetic consideration. Minimally invasive and breast-conserving approaches preserve both safety and appearance.
Learn more: Breast Surgery Services
Hand, Wrist & Upper Extremity Surgery
Restoring Function. Rebuilding Lives.
Injuries and conditions affecting the hand, wrist, or upper extremity can impact daily life. Endoscopic and minimally invasive techniques allow surgeons to repair these structures effectively.
Learn more: Hand, Wrist & Upper Extremity Care
Why Minimally Invasive Surgery Matters
Choosing a minimally invasive approach can mean:
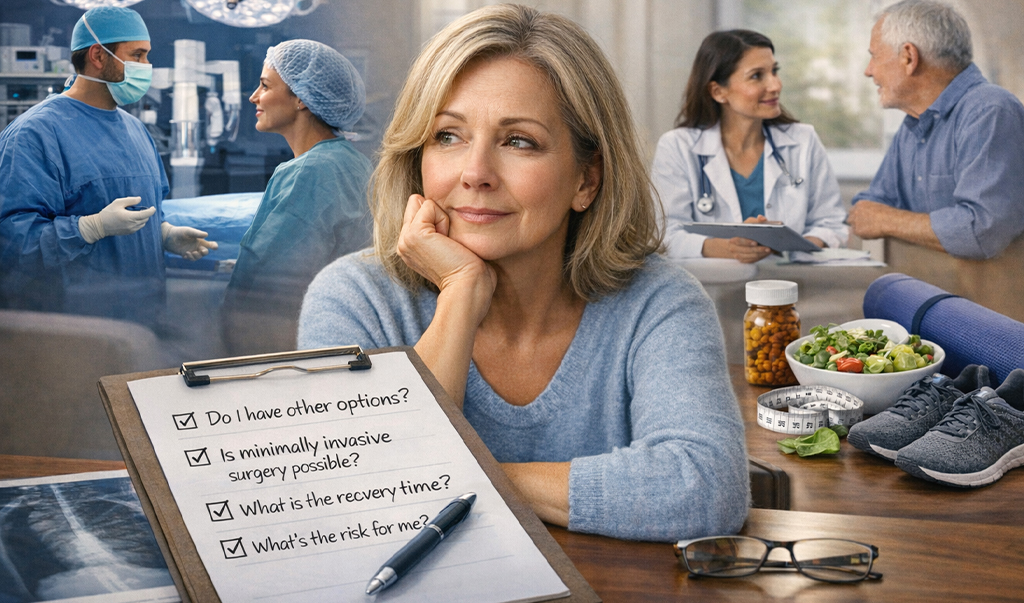
Our team evaluates each patient individually using advanced imaging, medical history, and comorbidity assessment to determine the safest approach.
Minimally Invasive Surgery vs. Traditional Open Surgery
While open surgery is still necessary in certain complex or emergency situations, minimally invasive surgery (MIS) is often the preferred approach.
| Aspect | Minimally Invasive Surgery | Traditional Open Surgery |
|---|---|---|
| Incisions | Small (0.5–1 cm), usually a few entry points | Large incision (6–12 inches) |
| Pain & Recovery | Less pain, faster recovery (days–weeks) | More pain, longer recovery (weeks–months) |
| Hospital Stay | Often outpatient or 1–2 days | Typically 5–7+ days |
| Infection Risk | Lower | Higher |
| Scarring | Minimal | Larger, visible |
| Precision | Enhanced via laparoscopic/robotic tech | Direct visualization only |
| Complication Rates | Generally lower | Higher in older/complex patients |
Bottom line: Minimally invasive surgery offers clear benefits in comfort, safety, and recovery. Open surgery remains essential when broader access is required for safety or complete treatment.
Patient-Centered Surgical Consent
Every patient receives comprehensive counseling:
Understanding your surgery is just as important as the surgery itself.
The Capital Surgeons Group Difference
Capital Surgeons Group combines decades of surgical expertise with the latest technology to provide high-quality, personalized care. From routine procedures like gallbladder removal to advanced robotic hernia repair, you can trust our surgeons to guide you safely through every step.
Surgery doesn’t have to be intimidating — it’s modern, precise, and patient-centered, emphasizing faster recovery, less pain, and better outcomes.
Ready to Take the Next Step?
Your journey to safer, less invasive, and more effective surgery begins today. Schedule a consultation with our expert surgeons to explore your options and discover how modern surgical techniques can improve your outcomes.
You May Also Like
Make an informed, confident decision about surgery by understanding your options, risks, recovery, and whether a non-surgical path may be right for you. [...]
Experience minimally invasive surgery at Capital Surgeons Group, combining advanced robotic and laparoscopic techniques for faster recovery and less pain. [...]
Capital Hand & Wrist Center, led by Dr. Jonathan Lundy, provides expert, compassionate care for hand, wrist, and upper extremity conditions in Austin. [...]
GLP-1 drugs offer non-surgical weight loss, while bariatric surgery provides lasting metabolic changes—we break down which option suits different needs. [...]
Discover how bariatric surgery offers 80% long-term success and can reverse chronic conditions like diabetes and sleep apnea. [...]
Understand how excess weight affects heart disease, life expectancy, and daily function—and how surgical treatment can change the trajectory. [...]
Learn why bariatric surgery offers lasting, life-changing weight loss and significant health benefits beyond medications. [...]
General Surgery: What You Need to Know
Transformative Solutions
for GERD
Explore in detail the advanced surgical options offered by our skilled surgeons at Capital Surgeons Group, highlighting the benefits of each procedure and emphasizing the precision, innovation, and patient-centric care that defines our approach. [...]
Why Choose Surgery
for Chronic GERD?
Discover why surgery might be the right choice for chronic GERD and explore advanced options. Learn about the limitations of non-surgical approaches and the benefits of choosing surgery for long-term symptom relief, reduced reliance on medications, and improved quality of life. [...]
Surgery vs. Long-Term Medication
Examine the downsides of prolonged use of heartburn medications, including the risks associated to dependency, and consider how surgical interventions present a more enduring solution to the fundamental problems. [...]
Laparoscopic Cholecystectomy
Explore the hidden details of laparoscopic cholecystectomy, a cutting-edge approach to gallbladder removal. Discover the benefits of this minimally invasive technique, and learn what to expect throughout your surgical journey. [...]
Da Vinci Robotic Cholecystectomy
Experience advanced care through Da Vinci Robotic Cholecystectomy, a cutting-edge solution leading the way in medical innovation. Ensuring precision and effectiveness, it stands at the forefront of treating Gallbladder Disease. [...]
Benefits of Cholecystectomy
Discover the transformative benefits of cholecystectomy, a surgical solution offering relief from gallbladder pain, prevention of recurrent gallstones, and improved digestive health. Explore the holistic enhancements to quality of life. [...]
Understanding
Gallbladder Disease
Discover the complexities of gallbladder disease and learn how Capital Surgeons Group stands out in its expertise, providing unparalleled understanding, precise diagnosis, and effective treatment for this widespread ailment. [...]
Cholecystectomy:
Gallbladder Removal Surgery
Advancements in surgical techniques have made cholecystectomy a highly effective treatment for gallbladder problems. Explore minimally invasive options like laparoscopic and robotic cholecystectomy for faster recovery and improved outcomes. [...]
Ventral Hernia and Treatment Options
Learn about ventral hernias, including their causes, symptoms, and treatment options. Discover the different types of hernia repair procedures and how to recover from surgery. [...]
Inguinal Hernia Treatment
Inguinal hernia, a common medical condition that can cause discomfort, pain, and other complications. Learn more about the causes, symptoms, and treatment options for inguinal hernia. [...]
Overcoming GERD
and Hiatal Hernia
Capital Surgeons Group specializes in the treatment of GERD, including minimally invasive surgery for hiatal hernia repair and the LINX procedure. Learn more about GERD surgery and its benefits for patients with chronic GERD symptoms. [...]